This post provides a guide to BPD Treatment and answers the questions: “What is BPD?” “What causes BPD?” “Is BPD genetic?” “Is BPD treatable?” and more. We’ll also cover the 9 BPD symptoms found in the DSM-5, therapy for borderline personality disorder and medication for borderline personality disorder.
Key Words
BPD or Borderline Personality Disorder: a mental illness that severely impacts a person’s ability to manage their emotions. This loss of emotional control can increase impulsivity, affect how a person feels about themselves, and negatively impact their relationships with others.
EUPD or Emotionally Unstable Personality Disorder: another name for BPD that emphasises the emotionally unstable aspect of the condition rather than the “borderline” aspect
DSM-5: a reference book on mental health and brain-related conditions and disorders. The American Psychiatric Association (APA) is responsible for the writing.
Neurotic: a propensity toward anxiety, negativity, and self-doubt.
Psychotic: a collection of symptoms that affect the mind, where there has been some loss of contact with reality.
Remission: a temporary diminution of the severity of disease or pain.
Recovery: a diminution of symptoms as well as improved psychosocial and vocational functioning.
Dysregulation: abnormality or impairment in the regulation of a metabolic, physiological, or psychological process.
Amygdala: a major processing centre in the brain for emotions, especially negative emotions such as fear, anxiety and aggression.
Serotonin: a chemical that carries messages between nerve cells in the brain and throughout your body. Serotonin plays a key role in mood.
Schema: describes patterns of thinking and behaviour that people use to interpret the world.
Transference: the redirection to a substitute, usually a therapist, of emotions that were originally felt in childhood.
Splitting: when a person sees everything as black or white, good or bad, or best or worst. Splitting is a defence mechanism people living with BPD use to deal with emotions (such as the fear of abandonment) that they cannot handle.
Systematic review: a review with a detailed and comprehensive plan and search strategy derived a priori, with the goal of reducing bias by identifying, appraising, and synthesizing all relevant studies on a particular topic.
Longitudinal studies: A study in which subjects are followed over time with continuous or repeated monitoring of risk factors / health outcomes.
Randomised Control Trial (RCT): A study in which a number of similar people are randomly assigned to 2 (or more) groups to test a specific drug or treatment. This reduces selection bias and increases reliability and validity of results.
What is BPD?

BPD or Borderline Personality Disorder is classified as a personality disorder, which are serious psychological conditions that can lead someone to persistently think, feel and behave in ways that deviate to cultural expectations. BPD, like most personality disorders, begins in adolescence or early adulthood and is characterised by pervasive instability in many areas of functioning. This can include a difficulty in managing emotions, controlling one’s behaviour, relating to others and building a sense of self. The threat of real or perceived abandonment or rejection is a common trigger for extreme outbursts that can include intense mood swings, extreme anger and impulsive behaviour.
BPD affects approximately 1.4% of the U.S. population, with 75% of cases being women, although recent research has suggested that the number of men with BPD may be higher due to misdiagnoses of PTSD and depression [1].
In a European and UK context, BPD is often referred to as Emotionally Unstable Personality Disorder or EUPD instead. This term, although interchangeable with BPD as they refer to the same underlying condition, places a greater emphasis on emotional instability, rather than ‘borderline’. This is due to borderline being considered by many an outdated label, based on the oversimplified belief in the mid 20th century that if patients did not fit neatly into either the “psychotic” or “neurotic” group, they must be borderline types [2].
Historically, BPD has been extremely stigmatised, with many healthcare professionals believing BPD treatment to be too difficult or unachievable. However this is a common myth as there is significant evidence to suggest that most patients respond well to BPD treatment and proceed to symptom remission, although less to full recovery. This means that someone with BPD does not have to live with the full extent of their symptoms forever and has the potential to live a high quality life.
Borderline Personality Symptoms
Symptoms for BPD or EUPD used by mental health professionals to diagnose the condition are listed in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), formulated by the American Psychiatric Association (this uses the term ‘Borderline Personality Disorder’), and the International Classification of Diseases (ICD-10), published by the World Health Organisation (which uses the term ‘Emotionally Unstable Personality Disorder’). Despite using different terms, both the DSM-5 and the ICD-10 list similar criteria, from which an individual must experience 5 or more symptoms to classify as having BPD.
The BPD DSM-5 advises 5 symptoms from the following list [3]: (these can be grouped into four categories of dysregulation; interpersonal, self, behavioural and emotional)
● Frantic efforts to avoid real or imagined abandonment.
● A pattern of unstable and intense interpersonal relationships characterised by alternating between extremes of idealisation and devaluation.
● Chronic feelings of emptiness.
● Identity disturbance: markedly and persistently unstable self-image or sense of self.
● Transient, stress-related paranoid ideation or severe dissociative symptoms.
● Impulsivity in at least two areas that are potentially self-damaging (e.g., excessive spending, high promiscuity, substance abuse, reckless driving, binge eating.)
● Recurrent suicidal behaviour, gestures, or threats, or self-mutilating behaviour.
● Affective instability due to a marked reactivity of mood (e.g., intense episodic dysphoria, irritability, or anxiety usually lasting a few hours and only rarely more than a few days).
● Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
Causes of BPD
Although there is no consensus over the causes of BPD, experts believe it most likely manifests due to a combination of genetic and environmental risk factors.
– Is BPD caused by childhood trauma?
History of abuse (physical, sexual, emotional) and neglect in childhood have been identified in up to 70% of people with BPD [4]. Trauma such as this can disrupt the formation of secure attachment between child and caregiver as well as distort perceptions of oneself and others, which can lead to a difficulty in forming stable relationships and a consistent and coherent sense of self when growing older – both core symptoms of BPD. Childhood trauma can also lead to individuals developing maladaptive coping strategies to deal with an overwhelming environment, which may account for the impulsive behaviour and extreme anger observed in patients with BPD.
– Is BPD Genetic?
Recent evidence suggests that up to 50% of the risk for BPD derives from a biological basis. Research using twin, family and adoption studies all suggest that there is a heritable component to BPD i.e. that individuals with a first-degree relative (such as a parent or sibling) with BPD, are at a higher risk of developing the disorder themselves as compared to the general population [5]. However in many cases a genetic vulnerability may not actually manifest into BPD without environmental stressors such as childhood adversity.
– Do people with BPD have different brain structure and function?
Neuroimaging studies indicate that certain brain regions of individuals with BPD are smaller and show differences in activity when compared to the general population. For example the amygdala (which regulates negative emotions such as anxiety, fear and aggression) of individuals with BPD showed significantly higher activity than the amygdala of a comparator control group (see figure 2) when shown the different facial expressions in figure 1 [6].
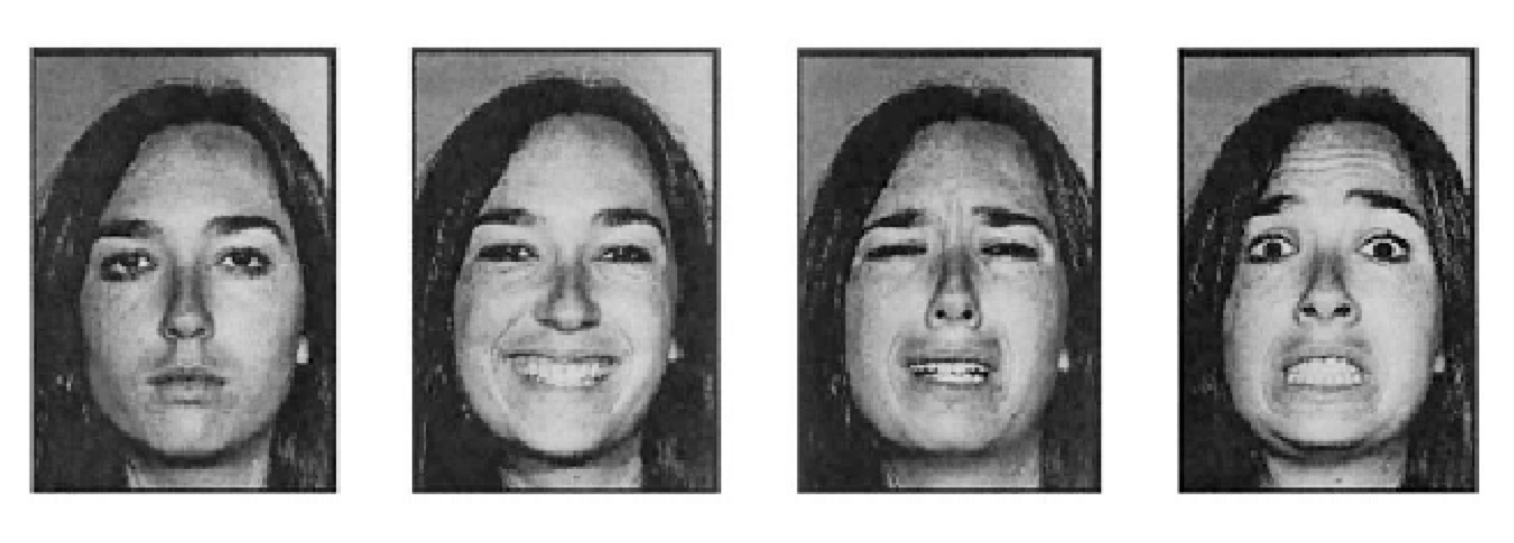
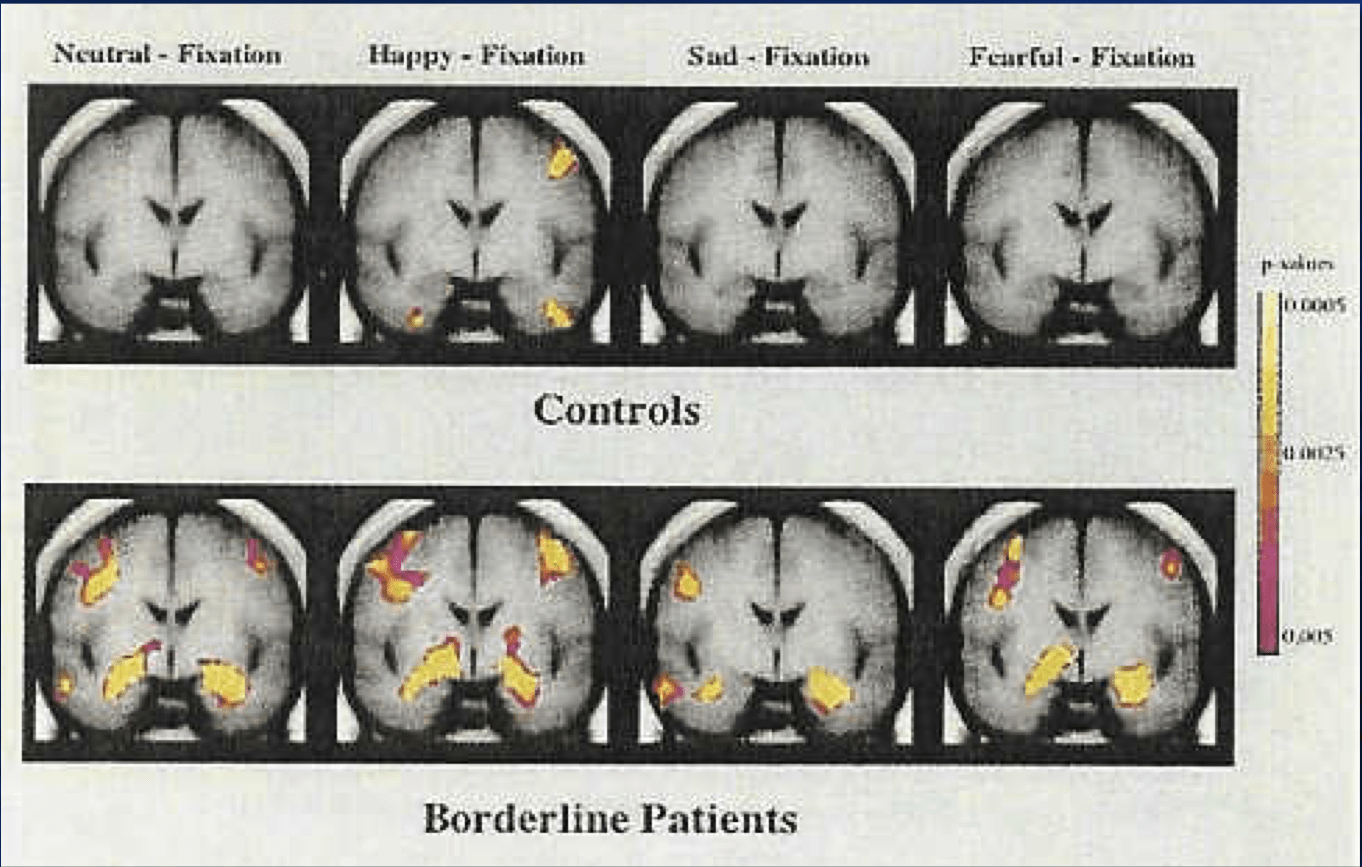
Figure 2: Two activation maps, demonstrating the difference in amygdala activity between BPD participants and healthy controls, in response to stimuli in figure 1. Highlighted areas (in pink and yellow) indicate activity. [6]
This overactivity may account for the impulsivity and extreme emotional reactions in people with BPD. Additionally, reduced serotonin function has also been observed in people with BPD, a neurotransmitter that plays a crucial role in mood stability. The development of brain structures can be influenced by environmental factors in childhood and so childhood adversity may contribute to brain structural and functional differences.
Is BPD Treatable?
It is important to remember that people with BPD have no choice over their condition and its symptoms. It is essential that they have access to the appropriate BPD treatment as their emotions and behaviours can become very hard to control without the correct support.
Psychological interventions are considered the first-line for BPD treatment. These can include psychodynamic treatments, that may focus on unconscious processes impacting emotions and behaviour or cognitive behavioural treatments that identify problematic thinking patterns and their connection to behaviour. Although there is no definite BPD cure, the consensus amongst experts is that engagement with psychological interventions is significantly more likely to lead to symptomatic remission and recovery from BPD when compared to no treatment groups.
Remission refers to the diminution of BPD symptoms to an extent that you would no longer meet the DSM-5 criteria for BPD. A systematic review involving 19 longitudinal studies and over 1000 patients, investigating the trajectory of symptoms post BPD treatment, showed that BPD remission, contrary to popular belief, is extremely common. Facilitating factors for remission included higher IQ, good childhood work history, good adult vocational history, low trait neuroticism and higher trait agreeableness [7]. Two cohorts that considered recurrence i.e. the return of symptoms after remission, found low evidence of it, suggesting that symptomatic remission is also stable over time [7]
One study reviewed was the McLean Study of Adult Development [8], which found that every 2 years of follow-up after treatment, the percentage of patients remitted significantly increased – up to nearly 82% after 10 years, as seen in the graph in figure 3. This has led some researchers to believe that increasing age can dampen the effects of BPD, for example via the diminution of impulsivity [7].
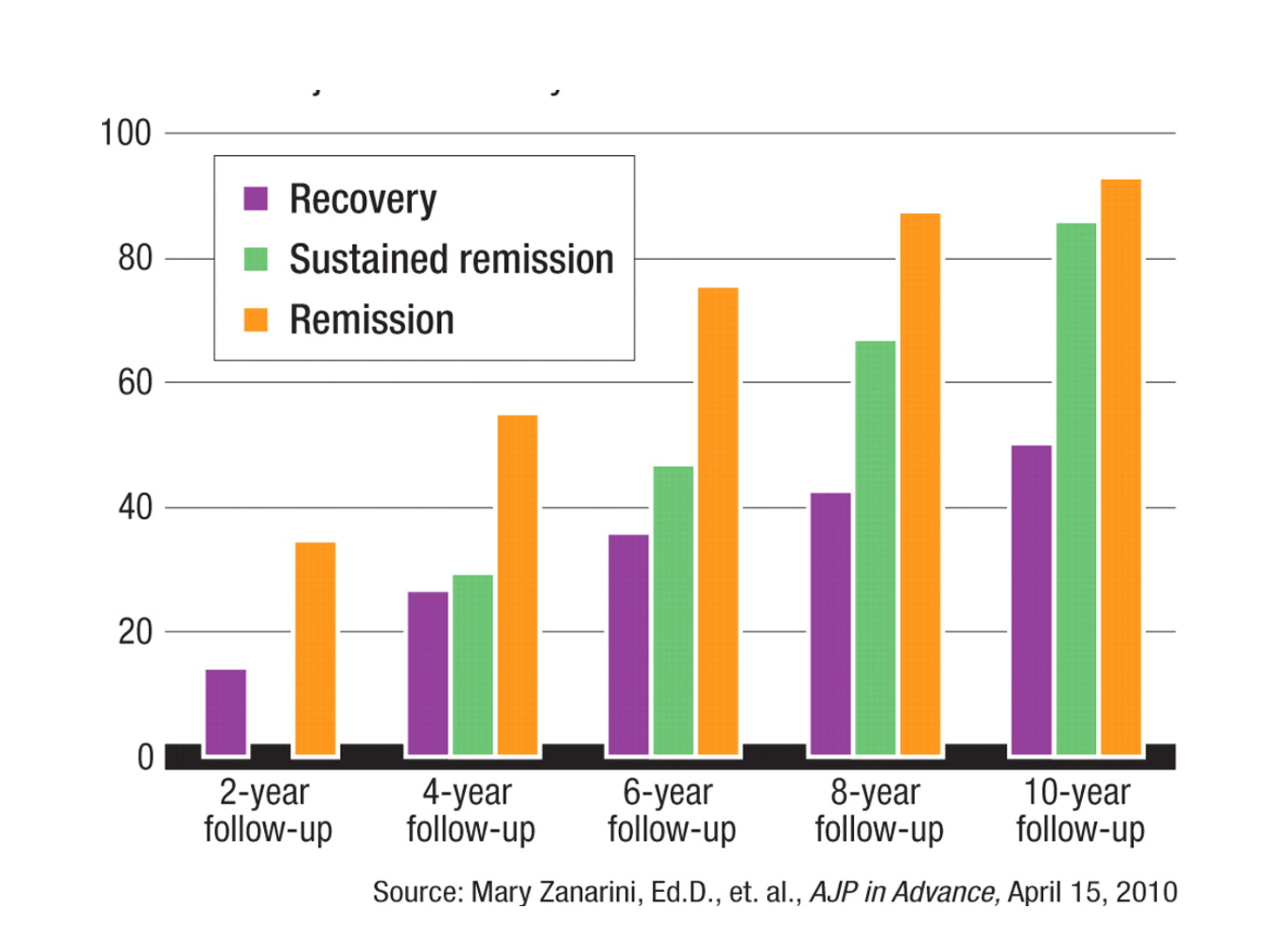
Recovery in the context of BPD treatment can be ambiguous, but refers generally to the idea that the individual has remission from symptoms and additionally is able to function well psychosocially and vocationally for extended periods of time, for example by maintaining a meaningful relationship and remaining consistently in employment. Longitudinal studies exploring the recovery rates of patients at 16 and 20 years post BPD treatment all found, like the 10 year study above, that 50-60% of individuals demonstrate recovery from BPD [9]. Facilitating factors for recovery included engagement with education or a vocation.
“Depression and bipolar disorder tend to remit quickly but recur much more often. Recovery from BPD is more akin to the process of maturation. It occurs slowly, but once you achieve a certain level, you stay there, and it takes some enormous stressor to push you back.” – Dr. Zanarini (author of McLean Study)
Recovery as compared to remission, is then a little more complex to achieve for people undergoing BPD treatment, however it is still stable over time, with around 30% relapsing [9]. To explain this
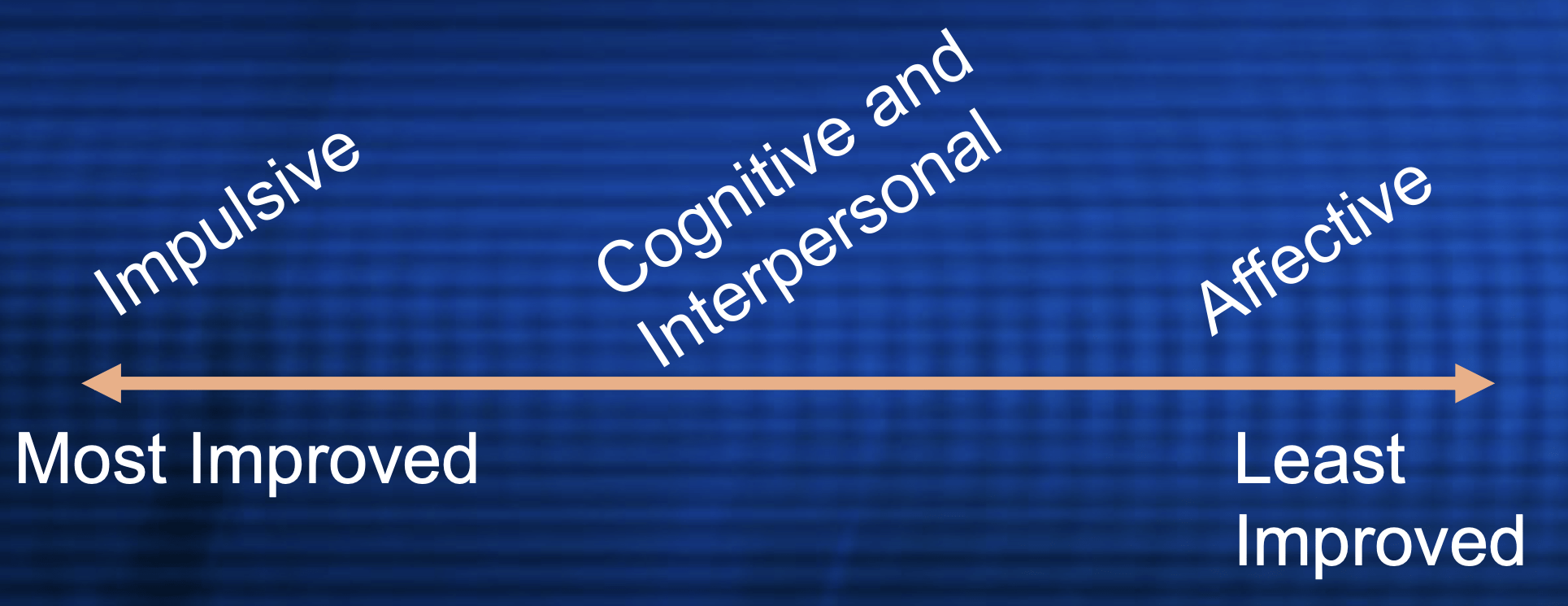
difference researchers looked at the finding in remission studies, that despite all symptoms reducing, this reduction was not equal across symptom domains, as seen in figure 4. Researchers thus theorised that although acute symptoms may remit quickly such as the self-harm related to impulsivity, symptoms such as extreme anger that fall under the affective i.e. emotional domain persist, impacting vocational and social success. Thus Dr Zanarini proposes a rehabilitation model of BPD treatment that incorporates training in life skills such as vocational training, to address the needs of those patients who can remit but not recover [9]. A consideration for co-morbid conditions such as depression, that may be contributing to the persistence of affective symptoms may also be useful to evaluate independently of BPD treatment, in order to increase chances of a full recovery.
Therapy for Borderline Personality Disorder
The type of BPD treatment involved in the remission and recovery studies above are specialised psychotherapeutic interventions such as Dialectic Behavioural Therapy (DBT), Mentalisation Based Therapy (MBT), Schema Focused Therapy (SFT) and Transferences Focused therapy (TFT).
Like many mental health illnesses, BPD symptoms manifest themselves on a spectrum and some people may experience one component of BPD more intensely than the other. Instead of taking a one size fits all approach, it is important to be informed about the different variations of therapy out there, each aimed at targeting different aspects of BPD:
| Therapy Type | Dialectic Behavioural Therapy | Mentalisation Based Therapy | Schema Focused Therapy | Transference Focused Therapy |
|---|---|---|---|---|
| BPD Target | Emotional vulnerability, intense guilt/worthlessness that comes after emotional outbursts, impulsive behaviour. | Unstable interpersonal relationships and splitting. | Maladaptive early schemas formed in childhood that lead to unhealthy coping strategies and behaviours. | Splitting, problematic interpersonal dynamics, intense emotional states and impulsive behaviour. |
| General Aims / Philosophy | Validation: accepting emotions are valid, real and acceptable Dialectics: most things in life are rarely “black or white”, it’s important to be open to ideas and opinions that contradict your own. | Mentalisation i.e. examination of own thoughts and beliefs as well as acceptance that one’s own interpretation of other people’s mental states may be incorrect. Clarification of misunderstandings. Emphasis on Interpersonal Relationships. Integration of Past Experiences. Promotion of Reflective Functioning. | To identify and change the deeply held thought and behaviour patterns i.e. schemas associated with patient’s past (usually those we cling to for emotional survival) | To prevent negative feelings about past experiences and people being transferred to current experiences and people. It is presumed that any feelings towards important people in the patient’s life will be transferred to the therapist. |
| Example | Therapist could accept (validate) that feelings of intense sadness cause an individual to self-harm, and that behaving in such a way does not make you a terrible and worthless person. However, the therapist would then attempt to challenge the assumption that self-harming is the only way to cope with feelings of sadness. The ultimate goal of DBT is to help an individual “break free” of seeing the world, relationships and life in a very narrow, rigid way that leads to engagement in harmful and self-destructive behaviour. | The therapist encourages the client to consider alternative perspectives, both their own and the other person’s. This promotes the development of mentalizing skills. For instance: Therapist: “How do you think your friend perceived the situation? What might have been going on in their mind? And how did your own thoughts and feelings influence your reactions?” | The therapist asks the patient about their core beliefs e.g. about themselves and others. Coping patterns will also be explored i.e.what is the patient’s pattern of behaviour in order to cope with these beliefs. For example, someone that believes deep down that they are truly unlovable due to childhood abuse, may engage in abusive relationships that reinforce these beliefs (i.e. surrender behaviour that reinforces existing beliefs) or repeatedly create conflict when they sense intimacy is forming (i.e. abandonment behaviour to avoid vulnerability). Therapist works to alter unhealthy coping styles that results from maladaptive schema by for example conducting exercises focused on venting anger, breaking unhealthy patterns of behaviour, and changing unhelpful ways of thinking. | The therapist may encourage the individual to express and articulate their feelings, thoughts, and perceptions when they are in the midst of splitting. They may also explore the roots of splitting behaviour back through to childhood as well as explore how the person’s feelings and attitudes toward the therapist reflect patterns from past relationships. |
| Evidence | Longitudinal studies have demonstrated that DBT is particularly effective in treating women with BPD who have a history of self-harming and suicidal behaviour. It’s been recommended by the National Institute for Health and Care Excellence (NICE) as the first treatment for these women to try. [10] | Randomized controlled trial of MBT in an outpatient setting (MBT-OP), with 134 patients randomly allocated to MBT or to a control, showed that those in the MBT group showed a steeper decline of both self reported and clinically significant problems, including suicide attempts and hospitalization. [11] | Patients randomly assigned to receive schema-focused therapy on top of ‘treatment as usual’ had significantly larger reductions in borderline personality disorder symptoms compared to patients assigned to just ‘treatment as usual’. [12] | A randomised control trial showed evidence for TFT being as effective as DBT in reducing thoughts of suicide, but better than DBT in reducing impulsive behaviours or anger. [13] |
A systematic review conducted in 2023, involving 54 randomised controlled trials found that when compared, there was no significant difference between each therapy type in addressing BPD treatment goals for patients i.e. they all showed equal evidence of effectiveness [14]. However as everyone with BPD has unique needs, it may still be useful to have a conversation with your healthcare professional about the different types of therapy available to help you decide if a particular one is more appropriate for you.
Furthermore this list is not exhaustive and there are many different types of treatment that do not follow traditional talk therapy principles. Click here to explore virtual EMDR.
Additionally for those who do not wish to work directly with a therapist, there are self-guided treatments available too, for example using a therapist recommended workbook, that can be followed at your own pace.
Medicine for Borderline Personality Disorder
Although not everyone with BPD requires medication as part of their treatment, the following types can be prescribed to target specific symptoms:
Antidepressants and Mood Stabilisers: These can include SSRIs, which can help with mood swings and dysphoria. Depakote can be used to aid with aggression.
Antipsychotics: Low doses of olanzapine for example can be used to control disorganised thinking or psychotic symptoms.
Anti-anxiety medications: Ativan, Xanax and Valium.
Research around effectiveness of drugs is mixed, while medication can be useful in a treatment plan (especially in conjunction with psychotherapy), some studies suggest certain drugs may make symptoms of BPD worse in particular individuals [15]. Also it is important to remember there is no “best” drug for BPD treatment, the right dose and type will depend on the individual’s symptoms and medical history, as well as a cost-benefit analysis of any potential side effects from taking the medication against BPD symptom alleviation. Therefore it is essential to have a discussion with your doctor before ever considering a prescription request in order to make the best decision for your health.
Additional Tips for BPD Treatment
Evidence unanimously points to the fact that BPD is not the life sentence it has historically been considered. However living and dealing with BPD is no easy feat and it is imperative that an individual has the right tools to help them cope. If you or someone you know is experiencing BPD symptoms or has recently been diagnosed with BPD here are some things you could do:
- Treating co-occurring conditions: Often those experiencing BPD have co-occurring conditions such as depression, PTSD, substance abuse and anxiety. Research suggests that these co-morbidities can contribute to poorer psychosocial outcomes, which reduces the likelihood of obtaining recovery from BPD [16]. Do not be afraid to mention more than one condition to your health care professional.
- Reducing stress: Being stressed can exacerbate symptoms and impact BPD treatment. It is important to identify sources of stress in your life and try to find ways to reduce them. In situations where reducing stress is not a viable option, learning relaxation techniques to cope with stress can be a very useful way to manage it. These might include deep breathing, exercise, visualization, and progressive muscle relaxation.
- Educate yourself. Take the time to learn about BPD so you can better understand what you or your friend/family member is going through. There are lots of myths floating around about BPD and research is always generating new recommendations so it is important to keep yourself informed.
- Develop coping skills: See more resources for BPD including books, 1-on-1 coaching, printables and other recovery content here that can help you form skills to deal with emotional distress and control impulsive behaviours. Research suggests that self-help measures can be more beneficial than professional interventions for BPD patients with strong internal motivation [16], so these are definitely worth a try!
- Involve your family. A diagnosis affects the whole family and often bpd treatment can be more successful if your family is involved.
- Find the right therapist for you. Therapy relies on trust, feeling safe and a genuine bond with the clinician. Even though most therapists are psychological experts and highly empathetic people, without this therapeutic alliance/bond, progress will not be made. Take the time to interview a few therapists to ensure they are a good fit for you and do not be afraid to request a referral if things aren’t working out after a few sessions. The Substance Abuse and Mental Health Services Administration also has an online treatment locator to help you find mental health services in your area. Additionally access to online therapy is available here.
- Join a community. Navigating BPD alone is definitely a challenge. Be sure to join our Facebook community here.
Some Useful Websites for more information on BPD treatment:
- National Education Alliance for Borderline Personality Disorder (NEABPD)
- National Institute of Mental Health
- McLean Hospital
- NAMI
- Mental Health America
References
- [1] https://www.nami.org/About-Mental-Illness/Mental-Health-Conditions/Borderline-Personality-Disorder
- [2] https://www.borderlinepersonalitytreatment.com/emotional-intensity-disorder.html
- [3] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3494330/
- [4] https://my.clevelandclinic.org/health/diseases/9762-borderline-personality-disorder-bpd
- [5] https://www.everydayhealth.com/bpd/borderline-personality-disorder-are-your-genes-blame/#:~:text=One%20strong%20predictor%20of%20the,50%20percent%20of%20your%20genes.
- [6] Donegan NH, Sanislow CA, Blumberg HP, Fulbright RK, Lacadie C, Skudlarski P et al (2003). Amygdala hyperreactivity in borderline personality disorder: implications for emotional dysregulation. Biol Psychiatry 54: 1284–1293.
- [7] Ng FYY, Bourke ME, Grenyer BFS. Recovery from borderline personality disorder: a systematic review of the perspectives of consumers, clinicians, family and Carers. PLoS One. 2016;11(8):e0160515.
- [8] Zanarini MC, Frankenburg FR, Reich DB, Fitzmaurice GM. Time to attainment of recovery from borderline personality disorder and stability of recovery: A 10-year prospective follow-up study. Am J Psychiatry. 2010;167:663–7.
- [9] Zanarini MC, Temes CM, Frankenburg FR, Bradford Reich D, Fitzmaurice GM. Description and prediction of time-to-attainment of excellent recovery for borderline patients followed prospectively for 20 years. Psychiatry Res. 2018;262:40–5.
- [10] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9396765/
- [11] Bateman A, Fonagy P. Randomized controlled trial of outpatient mentalization-based treatment versus structured clinical management for borderline personality disorder. Am J Psychiatry. 2009;166:1355–1364. [PubMed] [Google Scholar]
- [12] https://www.sciencedirect.com/science/article/abs/pii/S0005791609000020?via%3Dihub
- [13] Clarkin JF, Levy KN, Lenzenweger MF, Kernberg OF. Evaluating three treatments for borderline personality disorder: a multiwave study. Am J Psychiatry. 2007;164(6):922-8. doi:10.1176/ajp.2007.164.6.922
- [14] https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-022-04483-0
- [15]Dodds T. Prescribed benzodiazepines and suicide risk: A review of the literature. Prim Care Companion CNS Disord. 2017;19(2):16r02037. doi:10.4088/PCC.16r02037
- [16] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9237745/
BPD Resources
Learn more about Sadie’s Favorite – an upcoming novel about a woman with BPD. Manage your BPD symptoms with a printable workbook. Book an affordable coaching call with Audrey. See our recommended list of books about BPD. Download a free meditation app. Try a free trial of unlimited Virtual EMDR. Get 20% off your first month of online therapy with code THERAPY20 (financial aid options now available at checkout!).
Start a Discussion
Have you ever engaged with any form of BPD treatment? Share your experience in the comments!
Pin This Post
Liked this post? Please help support BPD Beautiful and spread BPD awareness by pinning it on Pinterest.